A study published in the Journal of Dental Research suggests a new system for classifying periodontal disease that may allow for earlier detection and personalized treatment before the disease becomes severe.
The researchers propose a new classification system – the first of its kind – based on the genetic expression of gum diseaseinstead of the current method based on clinical signs and symptoms.
They say such a system would enable earlier detection of gum disease, and allow individualized treatment, before teeth and bone loss sets in.
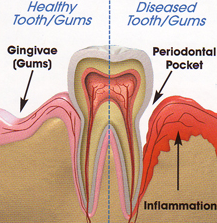
The present system, based on clinical symptoms, classifies periodontal disease as either “chronic” or “aggressive” depending on how swollen the gum is and how much bone is lost.
However, lead researcher, Panos N. Papapanou, professor and chair of oral and diagnostic sciences at the College of Dental Medicine at Columbia University Medical Center New York, NY, explains the problem with it:
“… there is much overlap between the two classes. Many patients with severe symptoms can be effectively treated, while others with seemingly less severe infection may continue to lose support around their teeth even after therapy.”
He says the problem is they cannot really tell when the gum infection is truly aggressive until the damage is severe and irreversible.
Researchers inspired by how genetic signatures are used to classify tumors
Spurred by the need for a better way to classify gum disease, the researchers looked at the recent changes to the way cancer is diagnosed.
Biologists are increasingly finding markers for cancer aggressiveness and responsiveness in the genetic signatures of tumors, and these are beginning to be used successfully to classify and select appropriate treatment for individual patients.
To establish whether such a model might work for gum disease, the researchers carried out a genome-wide analysis of diseased gum (gingival) tissue from 120 male and female patients aged from 11 to 76, diagnosed with either chronic or aggressive periodontitis.
They found each patient belonged to one of two clusters, depending on the genetic signature they found of their gum disease. Moreover, they found the two clusters did not align with the two classes of the current system based on symptoms, but they did differ with respect to extent and severity of the disease.
The patients whose gene signature put them in cluster 2 had much more serious gum disease.
Cluster 2 also contained patients with higher levels of infection of known oral pathogens, and there were more male than female patients in this cluster compared with cluster 1. This was in keeping with what we know about severe gum disease – that it is more common in men than women.
Molecular profiling could be basis of new system for classifying gum disease
Prof. Papapanou says the results indicate that molecular profiling offers a basis for a new classification system based on disease pathology that correlates well with how the disease presents clinically.
The new system could help spot patients with severe gum disease that has not yet shown clinical signs, he explains:
“If a patient is found to be highly susceptible to severe periodontitis, we would be justified in using aggressive therapies, even though that person may have subclinical disease. Now, we wait years to make this determination, and by then, significant damage to the tooth-supporting structures may have occurred.”
He and his team now want to carry out a study where they use the new classification system with a group of patients that they follow to see how well it predicts disease outcomes.
They also want to find a way to typify the two clusters with biomarkers instead of genes, because they would be much easier to look for (for instance by analyzing molecules present in gum samples) than having to perform genome-wide tests on each patient.
Medical News Today recently learned of a paper published in the Australian Dental Journal that exploredepigenetics and oral health. There, researchers from the University of Adelaide’s School of Dentistry, say epigenetics has much to offer in the future treatment and prevention of dental disease, and predict that one day a visit to the dentist may well involve looking at how the patient’s genes are being switched on and off.
Written by Catharine Paddock PhD
http://www.medicalnewstoday.com/articles/274458.php